
Sinaptica On Precision Neuromodulation To Combat Alzheimer’s: ‘No Drug Dares Go After Moderate Patients’
by Ryan Nelson
CEO Ken Mariash and scientific co-founder Giacomo Koch discuss plans for a Phase 3 trial in 2025 supporting Sinaptica’s combination of transcranial magnetic stimulation, electroencephalography and machine learning to slow Alzheimer’s progression. Potential synergies with anti-amyloid drugs, reflections on the US FDA’s TAP program, and insight into the company’s machine learning capabilities.
Sinaptica Therapeutics is gearing up for a Phase 3 trial in mid-2025 of its neuromodulation therapy that it believes could benefit Alzheimer’s patients beyond pharmaceuticals’ reach.
Designated a Breakthrough Device by the US Food and Drug Administration, Sinaptica’s system combines repetitive transcranial magnetic stimulation (TMS) targeting the precuneus – a “key node” of the default mode network that’s responsible for episodic memory – with electroencephalography monitoring and machine learning to offer a non-invasive precision therapy, the company says.
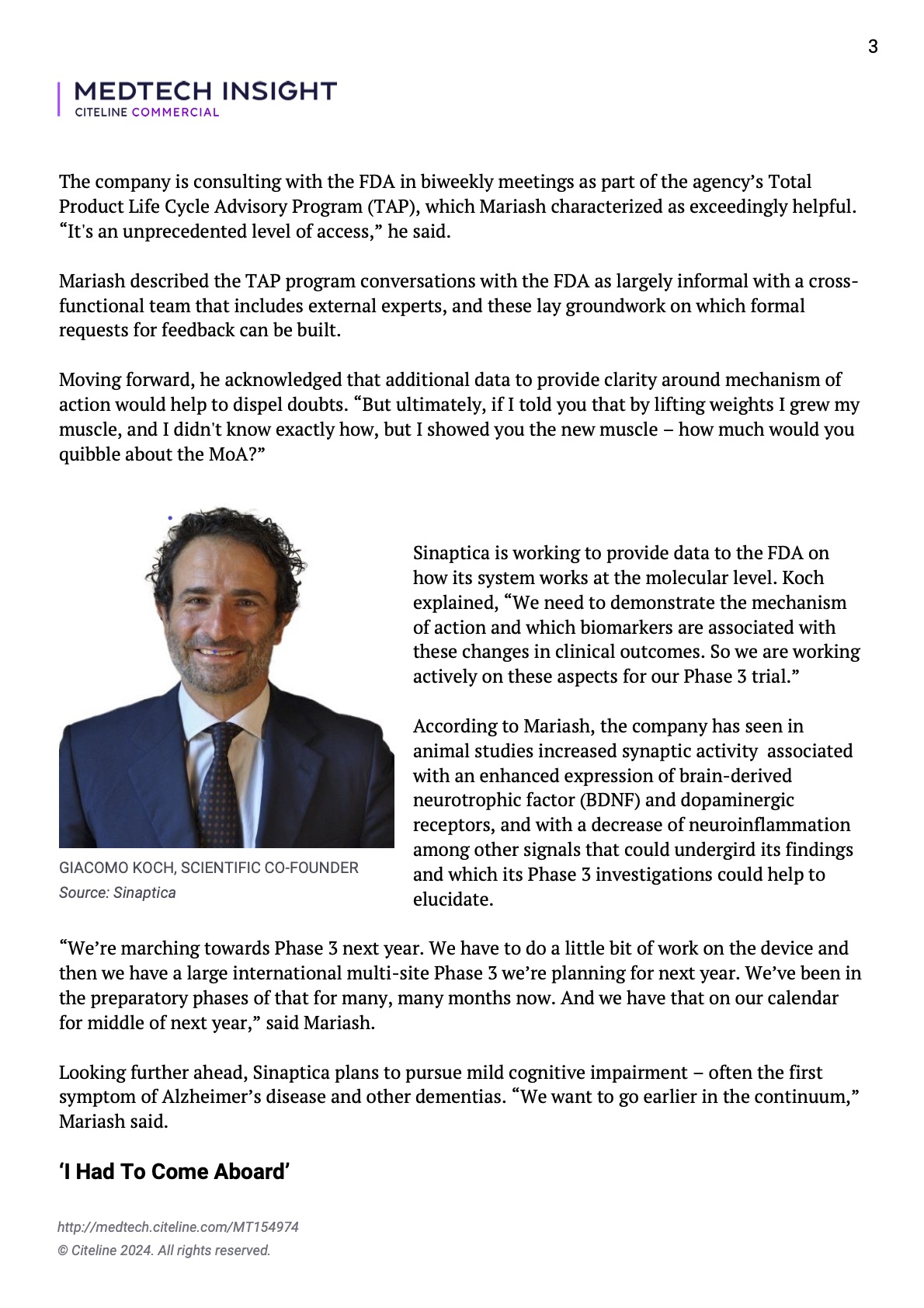
Giacomo Koch, Sinaptica’s scientific co-founder, full professor of Human Physiology at University of Ferrara, and head of the non-invasive brain stimulation lab at the Santa Lucia Foundation in Rome, Italy, will be presenting the results of a new Phase 2 study on 31 October at the CTAD Alzheimer’s Conference in Madrid, Spain.
The results build on already published Phase 2 data in the journal Brain that link Sinaptica’s approach to greater than 80% slowing of clinical endpoints for disease progression in mild to moderate Alzheimer’s cases after six months of treatment. Coming data from the second Phase 2 (with previous and new patients) will describe clinical effects using the same protocol in a randomized blinded fashion after one year of treatment.
On a pilot scale, the company co-founders also have demonstrated via magnetic resonance imaging (MRI) grey matter preservation and, via fMRI, increased functional connectivity in Alzheimer’s patients treated with personalized therapy versus a sham treatment arm. (Also see “Sinaptica’s Breakthrough Device Could Slow Brain Atrophy In Alzheimer’s Patients – Study” – Medtech Insight, 10 Jul, 2024.)
“A lot of it, to my mind, is helping satisfy the doubters,” said Sinaptica CEO Ken Mariash in a 12 July interview with Medtech Insight. “Despite having nailed all relevant endpoints, there are still the doubters who are like, ‘That’s just a single study.’ So to have a second study done now is great because it will show tremendous results as well.”
Importantly, Mariash said, “these are the toughest patients. No drug is daring to go after moderate patients – they’ve all failed. So these patients are thought of as almost ‘beyond the pale’ as far as ability to treat them. And yet we’re able to slow the disease by a clinically meaningful extent.”
Going forward, Cambridge, MA-based Sinaptica is committed to reaching patients earlier in the disease continuum. “It’s kind of like cancer – why wait until it gets to stage two? You want to get it as early as possible. With the advent of blood-based biomarkers and new service lines meant to identify patients and diagnose them as early as possible, we see the possibility now of being able to treat patients earlier and earlier.”
In Mariash’s view, Sinaptica has produced promising evidence of disease modification across numerous imaging and electrophysiology endpoints.
The company is consulting with the FDA in biweekly meetings as part of the agency’s Total Product Life Cycle Advisory Program (TAP), which Mariash characterized as exceedingly helpful. “It’s an unprecedented level of access,” he said.
Mariash described the TAP program conversations with the FDA as largely informal with a cross- functional team that includes external experts, and these lay groundwork on which formal requests for feedback can be built.
Moving forward, he acknowledged that additional data to provide clarity around mechanism of action would help to dispel doubts. “But ultimately, if I told you that by lifting weights I grew my muscle, and I didn’t know exactly how, but I showed you the new muscle – how much would you quibble about the MoA?”
Sinaptica is working to provide data to the FDA on how its system works at the molecular level. Koch explained, “We need to demonstrate the mechanism of action and which biomarkers are associated with these changes in clinical outcomes. So we are working actively on these aspects for our Phase 3 trial.”
According to Mariash, the company has seen in animal studies increased synaptic activity associated with an enhanced expression of brain-derived neurotrophic factor (BDNF) and dopaminergic receptors, and with a decrease of neuroinflammation among other signals that could undergird its findings and which its Phase 3 investigations could help to elucidate.
“We’re marching towards Phase 3 next year. We have to do a little bit of work on the device and then we have a large international multi-site Phase 3 we’re planning for next year. We’ve been in the preparatory phases of that for many, many months now. And we have that on our calendar for middle of next year,” said Mariash.
Looking further ahead, Sinaptica plans to pursue mild cognitive impairment – often the first symptom of Alzheimer’s disease and other dementias. “We want to go earlier in the continuum,” Mariash said.
‘I Had To Come Aboard’
Speaking to Sinaptica’s initial Phase 2 data published in Brain, Mariash said, “When I saw that data, I knew I had to come aboard.”
Before being appointed CEO of Sinaptica in May 2023, Mariash served in leadership roles including director, strategy and new markets, for Boston Scientific’s nearly $1bn neuromodulation division, and strategy and business development manager at Baxter BioScience, now part of Takeda.
“For 20 years, I’ve been monitoring the space,” Mariash said. “In 2004, we at Baxter had a Phase 3 study in Alzheimer’s and – spoiler alert – it failed, like dozens of other studies. When I saw this [Sinaptica] data, I said, ‘Wow, this is totally different. It’s a bright-line signal of over 80% slowing across every endpoint.’”
Personalization is central to Sinaptica’s approach. Koch noted, “Every patient has a different degree of connectivity as well as degree of impairment.”
Patients also respond differently to TMS. The challenge is to stimulate the right point in the precuneus with the right amount of intensity so that it safely activates the entire default mode network.
Mariash explained, “You can’t just carpet-bomb the brain and hope that you get the right response. If we’re off by even a centimeter, we can hit the wrong network – we could hit the dorsal attention network, for example, which anti-correlated with the default mode network. Intensity also has to be dialed in. We want to see strong propagation but not too much. There is a theoretical risk of a seizure, though we have both to personalize our therapy and to ensure a safe maximum dose.”
Once the calibration is complete and the data are thoroughly analyzed for optimal target engagement, the patient undergoes at least three months of 20-minute sessions – at first daily and, after two weeks, weekly – before recalibration.
“There was no recalibration in the original Phase 2. We plan to do that going forward because we think recalibration is an essential part of optimizing efficacy and potential durability of the therapy,” Mariash said.
Sinaptica and its algorithms will continue to benefit from the wealth of TMS-EEG data that Koch has amassed at Santa Lucia Foundation’s brain stimulation lab (see box), as well as from future clinical studies. Koch noted his additional work exploring TMS-EEG to treat not only Alzheimer’s, but also stroke, Parkinson’s, and traumatic brain injury. “And then there is a big, big space, we think, in developmental disorders, autism spectrum disorder, that’s also very related,” he said.
Complementary To Drugs
Sinaptica does not consider itself in competition with anti-amyloid drugs, namely Eli Lilly and Company’s recently approved donanemab (Kisunla) and Eisai and Biogen’s lecanemab (Leqembi).
“We applaud these new approvals,” Mariash said. “They do statistically significantly slow the disease … and this is a great achievement for the space.”
At the same time, with regard to donanemab, “patients come off the drug after they’ve cleared the amyloid. It is not clear at all what they do after. So I think it makes perfect sense to add a complementary therapy at that point, or together upstream. If physicians want to combine our therapy with drugs like donanemab and lecanemab, that could be a very synergistic possibility.”
Koch, who served on Roche’s global advisory board and has led several clinical trials including one recently funded by the Alzheimer’s Drug Discovery Foundation on the drug rotigotine’s effects in Alzheimer’s patients, agreed.
“Everyone out in the field understood after these big trials with anti-amyloid drugs that it’s not possible that a single compound will be sufficient. So everyone now is talking about combination therapy; the analogy is with cancer. And our approach comes from another perspective, has no side effects, and could be combined with potentially any drug. And we have to consider that many patients will not be prescribed these new anti-amyloid drugs or even new drugs coming into the market in the near future because of label limitations and side effects,” Koch said.
As for competing devices in development to treat Alzheimer’s, such as Cognito Therapeutics’ Spectris headset and NeuroEM Therapeutics’ MemorEM, both FDA-designated Breakthrough Devices as well, Mariash said, “We welcome every approach.”
He added, “This space demands that we look at Alzheimer’s from fresh and new and bold perspectives – we have to come at this from every angle.”
Mariash acknowledged that neuromodulation is not universally well-known or broadly clinically adopted beyond some specific indications. “But it is a $7 billion space that has transformed many disease states, whether it’s Parkinson’s, or epilepsy, or overactive bladder, or pain, or in the case of Setpoint [another FDA Breakthrough Device sponsor] rheumatoid arthritis potentially, the biggest drug class after COVID vaccines. So we see the transformative potential of neuromodulation in so many places including Alzheimer’s, and where the field is going is precision medicine, closed loop approaches, combined with a connectome-based personalized approach.”
Sinaptica’s ML
On AI, Mariash said, “I like to use the word machine learning instead of AI, because AI implies that the machine is figuring out and changing as it goes. That creates some challenges with the FDA that are not applicable to our therapy. So machine learning is a method to develop algorithms by training on datasets. And Giacomo has got amazing access to training data and has amassed this huge database from TMS-EEG recordings, not only in Alzheimer’s patients, but others. So if you use that data and other data to train our algorithms, as we did, you come up with algorithms that are explainable to FDA and aren’t a complete black box.”
He continued, “Now the data that we generate is massive and noisy, so we have to use cleaning algorithms to go through and clean and normalize the data. We’ve got some NASA signal processing engineers working on that. It’s not trivial. You’ve got eye blinks, you’ve got motion artifacts, you’ve got startle responses, you’ve got scalp contact issues, it’s a really tough problem to get it to an analyzable state. And then once you have the data clean, you have to feature-extract, you have to know what to look for. There’s hundreds and hundreds of features in the data; you don’t know what to look for unless you’ve done the research to know which features matter. So we’ve done the research, we know what to look for, and we’ve developed and trained our algorithm based on that. And it will constantly improve – the more data we get, the more we learn, and every patient that sits in that chair and does our evaluation is more information that we can use to optimize the therapy – and learn more about Alzheimer’s.”
About Sinaptica Therapeutics
Sinaptica Therapeutics is a clinical-stage neuromodulation therapeutics company leading the development of a new class of personalized therapeutics to revolutionize the treatment of Alzheimer’s and neurodegenerative diseases. The company utilizes a novel, noninvasive approach to treating Alzheimer’s via precision neurostimulation of a key brain network involved in memory, the Default Mode Network. This novel approach slowed disease progression by >80% on all four gold-standard cognitive and functional clinical endpoints in a placebo-controlled Phase 2 clinical study, with results published in the peer-reviewed Oxford University Press journal, Brain. The technology was granted Breakthrough Device Designation by the FDA in 2022 and the company is preparing for a pivotal randomized controlled clinical trial in early 2025. Sinaptica’s mission is to bring a safe, effective, and noninvasive neuromodulation therapy to Alzheimer’s patients that can help to significantly slow the progression of both cognitive and functional decline. Learn more at sinapticatx.com and follow us on LinkedIn and Twitter @SinapticaTX.
The SinaptiStim™ System is for investigational use only. It has not been approved by the U.S. Food and Drug Administration and is not available for commercial sale in any geography.
Media contact:
Kathryn Morris, BrightPoint
kathryn@brightpointny.com
914-204-6412